In the spirit of Raistlin’s post, I’m also not starting a new game but I wanted to see what I could do with Evennia and nWoD/Chronicles of Darkness. See, I kind of dislike oWoD and am not entirely sure why it’s currently in the zeitgeist to run on WoD MUSHes (with the exception of City of Glass most recently). I could go into why that is, but that’s not the intention of this post.
Okay! So PyReach is intended to be a setting-neutral and system-focused Chronicles of Darkness (or nWoD 2nd Edition) code system. It’s not remotely ready, but I do have a public repo for it. One day if I figure it out (or ask other, better python coders I know very nicely) I’ll set up an installer file for super ease of use.
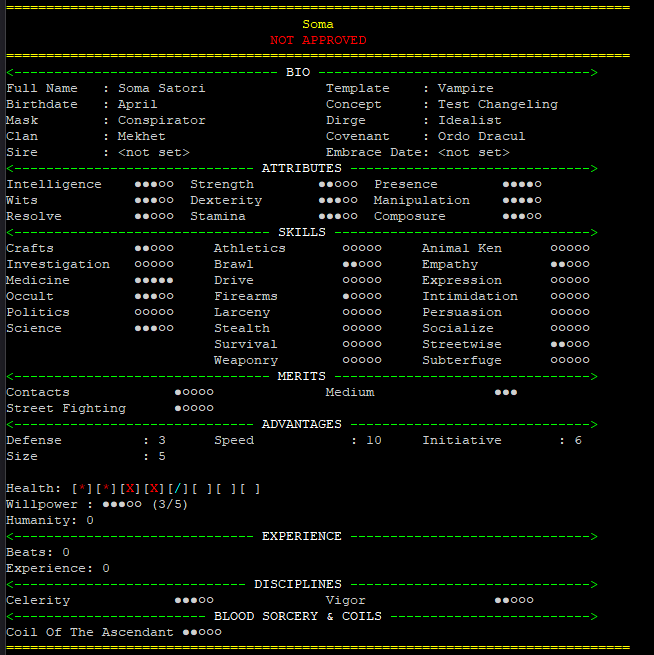
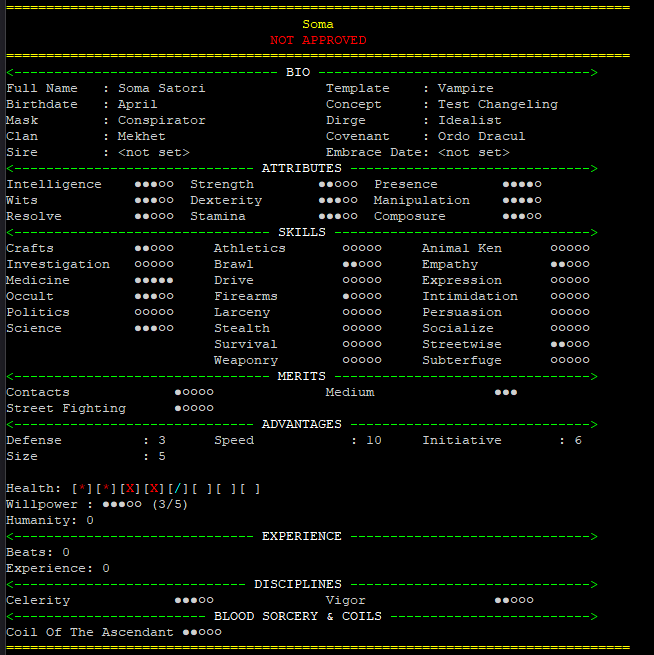
Someone once told me that all you need to get a game started is a sheet and a rolling system. Well, we got that!
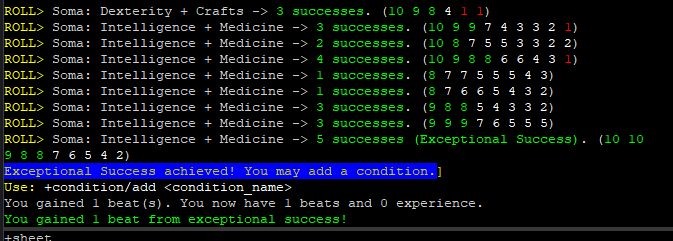
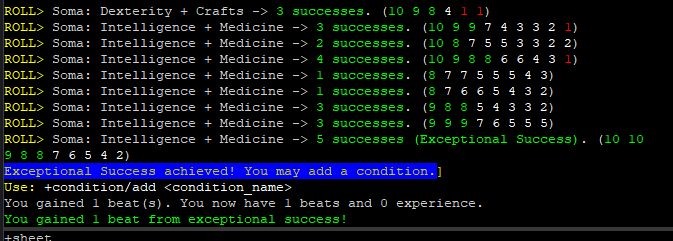
Excuse the dice spam, I was trying to get an exceptional success:
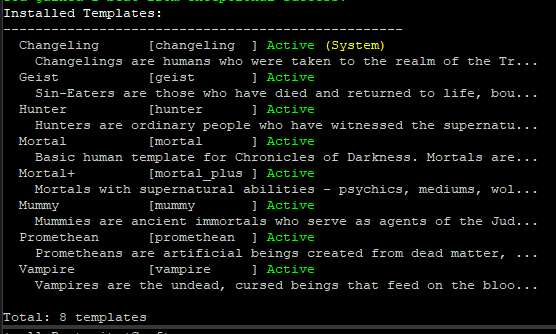
Mainly it’s a modular system. Because I don’t have a particular game in mind (though I have some ideas, but I don’t really have time to run anything), I set everything up to be templates and modules that you install into the system. For example:
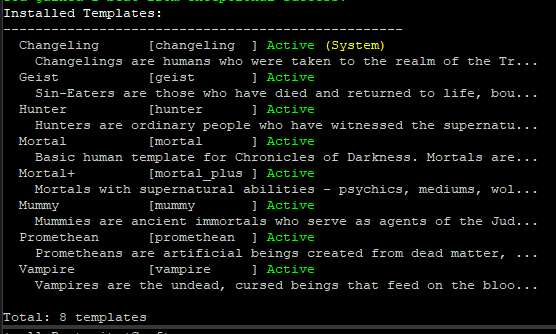
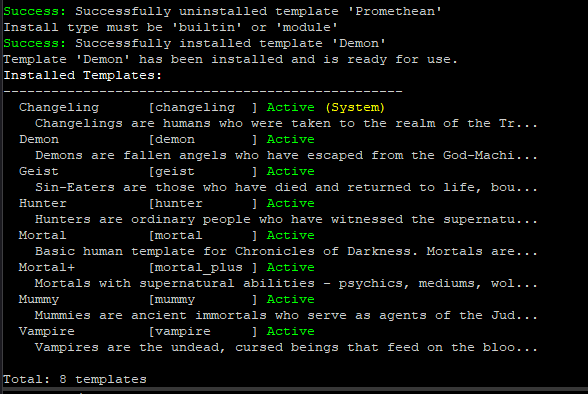
If something is marked “System” it means you have indicated that it cannot be uninstalled. If I wanted to, for instance, uninstall Promethean and then install Demon, it would look like this:
(ignore my own syntax error there)
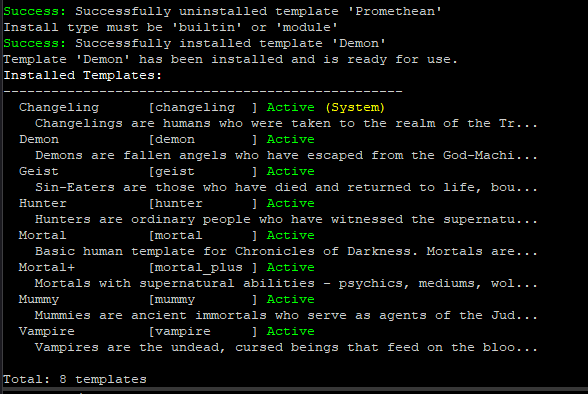
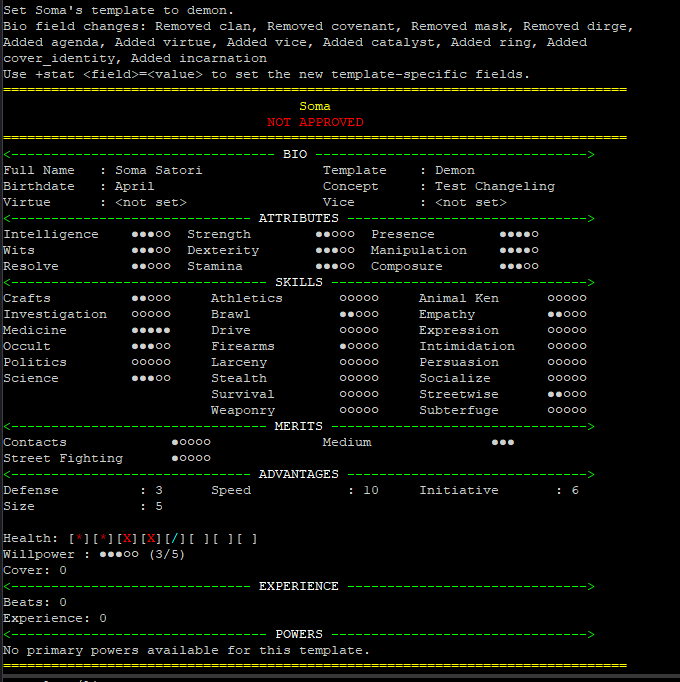
Demon isn’t really set up, as in I haven’t really entered any of the powers or anything into the system, but now we can change our character sheet over to Demon and it’ll update our bio information and clear out the section that shows our vampire-specific powers. the sheet code doesn’t know to look for Catalyst, Agenda, Ring, Cover Identity, or Incarnation, so it will ignore that in favor of the vanilla mortal stuff.
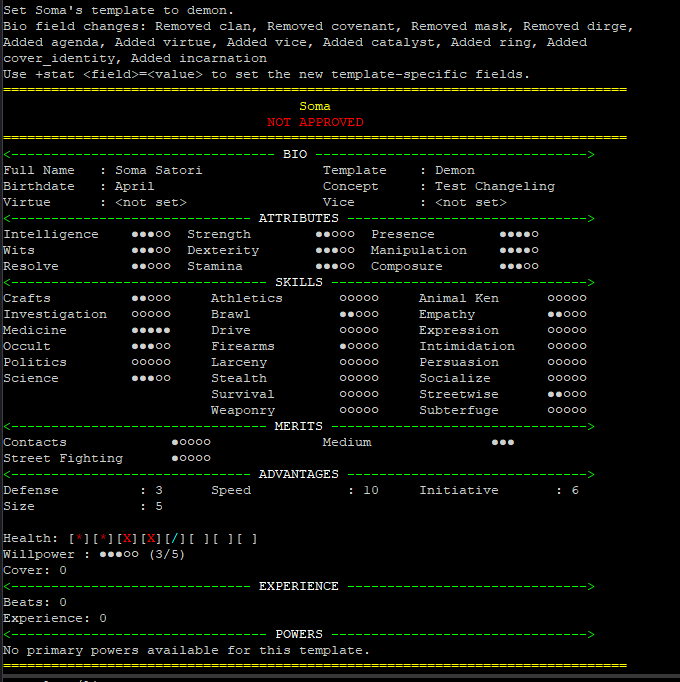
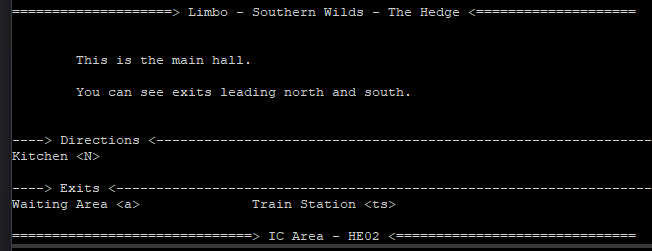
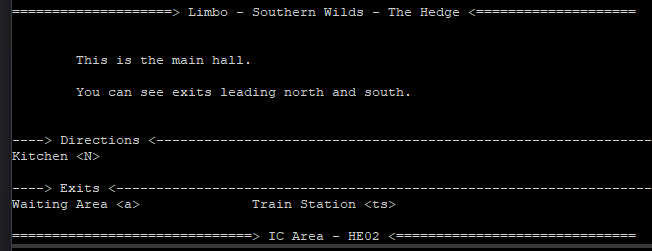
Let’s see… other stuff. Health is in there, as you can see it updates live on the sheet. I’m still working out the kinks about getting it to subtract a health penalty. Spending & regaining WP is set up, but I haven’t set that up for other power points like Vitae or Glamour. I have a rudimentary room template based on the way The Reach (and Fallcoast) rooms look:
and… yeah! Still working on it, no idea when it’ll be done. It’s a hobby project. There’s some other stuff, but it’s probably not as interesting as these more essential pieces.